Early Signs of Diabetes and Tips to Manage Blood Sugar

Diabetes is a chronic health condition that affects how your body processes glucose, a vital source of energy. With millions of people diagnosed worldwide, diabetes has become a pressing health issue. Early detection and management are crucial to preventing complications and ensuring a healthy life. This article explores the early signs of diabetes, risk factors, and practical tips to manage blood sugar effectively.
What Is Diabetes?
Diabetes occurs when the body is unable to properly regulate blood sugar levels. This happens either because the body does not produce enough insulin, a hormone that helps glucose enter cells, or because the body cannot effectively use the insulin it produces.
There are three main types of diabetes:
1.Type 1 Diabetes: An autoimmune condition where the body attacks insulin-producing cells in the pancreas. It often develops in childhood or adolescence but can occur at any age.
2.Type 2 Diabetes: The most common form, typically linked to lifestyle factors and insulin resistance. It often develops in adults but is increasingly seen in children.
3.Gestational Diabetes: A temporary condition that occurs during pregnancy and increases the risk of developing Type 2 diabetes later in life.
Recognizing the early signs of diabetes can help individuals take action before the condition worsens.
Early Signs of Diabetes
1. Frequent Urination (Polyuria)
One of the earliest signs of diabetes is increased urination. High blood sugar levels cause the kidneys to work overtime to filter and remove excess glucose through urine. If you notice that you're visiting the bathroom more frequently, especially at night, it could be a warning sign.
2. Excessive Thirst (Polydipsia)
Frequent urination can lead to dehydration, which triggers an intense feeling of thirst. If you find yourself drinking more water than usual without clear cause, it may be linked to high blood sugar levels.
3. Unexplained Weight Loss
People with diabetes often experience sudden and unintentional weight loss. When the body cannot use glucose for energy, it starts breaking down fat and muscle instead, leading to weight loss. This is more common in Type 1 diabetes but can also occur in advanced Type 2 diabetes.
4. Fatigue
Feeling constantly tired or fatigued is another common symptom. When cells cannot absorb glucose effectively, the body lacks the energy it needs, leaving you feeling drained.
5. Blurred Vision
High blood sugar can cause fluid to accumulate in the lenses of the eyes, leading to blurred vision. If left untreated, it can result in long-term damage to the eyes, including diabetic retinopathy.
6. Slow Healing of Wounds
High blood sugar impairs circulation and affects the body’s ability to heal wounds. If cuts or sores are taking much longer to heal than usual, it’s important to get checked for diabetes.
7. Frequent Infections
Diabetes can weaken the immune system, making the body more prone to infections, such as urinary tract infections (UTIs) or yeast infections. These may be recurring and harder to treat.
8. Numbness or Tingling in Hands and Feet
Nerve damage, or neuropathy, is a common complication of diabetes. Early signs include numbness, tingling, or a "pins and needles" sensation in the extremities.
Risk Factors for Developing Diabetes

Several factors increase the likelihood of developing diabetes:
Obesity or being overweight: Extra weight, especially around the abdomen, increases insulin resistance.
Sedentary lifestyle: Lack of physical activity contributes to weight gain and poor glucose metabolism.
Family history: A close relative with diabetes increases your risk.
Age: The risk of Type 2 diabetes increases after age 45.
Pre-diabetes: Elevated blood sugar levels that are not yet high enough for a diabetes diagnosis.
Gestational diabetes history: Women who had diabetes during pregnancy are at a higher risk of developing Type 2 diabetes.
Tips to Manage Blood Sugar
Managing blood sugar is essential for those with diabetes or at risk of developing it. Here are practical tips to keep your blood sugar levels in check:
1. Healthy Eating Habits
A balanced diet is crucial for managing blood sugar.
Focus on nutrient-dense foods like vegetables, whole grains, lean proteins, and healthy fats.
Incorporate high-fiber foods to slow glucose absorption and prevent spikes in blood sugar
Avoid sugary and processed foods, which can cause rapid blood sugar increases.
Portion control is key—eating smaller meals throughout the day can help maintain stable blood sugar levels.
2. Regular Exercise
Physical activity helps your body use insulin more effectively.
Aim for at least 150 minutes of moderate exercise per week, such as walking, jogging, or swimming.
Strength training twice a week can improve muscle mass and insulin sensitivity.
Find activities you enjoy to make exercise a regular part of your routine.
3. Maintain a Healthy Weight
Excess weight is a significant risk factor for Type 2 diabetes.
Losing even 5–10% of your body weight can make a big difference in blood sugar control.
Combine diet and exercise for sustainable weight loss rather than relying on extreme diets.
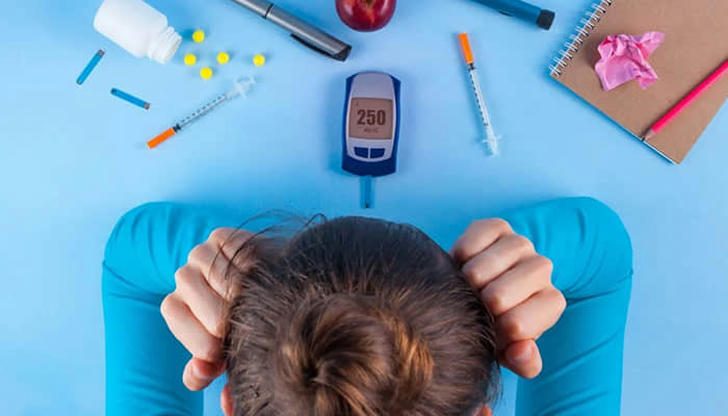
4. Monitor Blood Sugar Levels
Regular monitoring helps track how your lifestyle choices affect your blood sugar.
Use a glucometer or continuous glucose monitor (CGM) as recommended by your healthcare provider.
Keep a log of your readings to identify patterns and make adjustments as needed.
5. Stay Hydrated
Drinking water helps the kidneys flush out excess glucose from the body.
Aim for at least 8 glasses of water a day.
Avoid sugary drinks like soda and fruit juice, which can cause blood sugar spikes.
6. Medications and Insulin Therapy
For some people, lifestyle changes alone may not be enough to manage blood sugar.
Oral medications can help improve insulin sensitivity or reduce glucose production.
Insulin therapy may be necessary for individuals with Type 1 diabetes or advanced Type 2 diabetes.

- Stress Management
Stress hormones like cortisol can raise blood sugar levels.
Practice relaxation techniques such as meditation, yoga, or deep breathing exercises.
Find time for hobbies and activities that help you unwind.
Ensure you’re getting enough sleep to support overall health and stress reduction.
- Regular Check-ups
Schedule routine visits with your healthcare provider to monitor your progress.
Important tests include the HbA1c (average blood sugar levels over 3 months) and lipid profile to assess cholesterol levels.
When to Seek Medical Help
Seek medical attention if you experience symptoms of extremely high or low blood sugar, such as:
Severe headaches.
Confusion or difficulty concentrating.
Rapid heartbeat or sweating.
Loss of consciousness.
Early intervention can prevent complications and improve your quality of life.
Conclusion
Diabetes is a serious but manageable condition. By recognizing the early signs and making proactive lifestyle changes, you can take control of your health. A healthy diet, regular exercise, and stress management are foundational steps to keeping blood sugar levels stable. For those already diagnosed, regular monitoring and adherence to a treatment plan are essential. Remember, early action can make a significant difference in preventing complications and living a healthier life.
